Gli esperti avvertono che i superbatteri potrebbero uccidere milioni: azioni intraprese contro la resistenza ai farmaci
Meta Description
Millions of deaths could result from antibiotic-resistant super bugs by the year 2050. Learn about the intraprese actions and challenges that the experts face in order to counteract the antimicrobial resistance.
Introduction
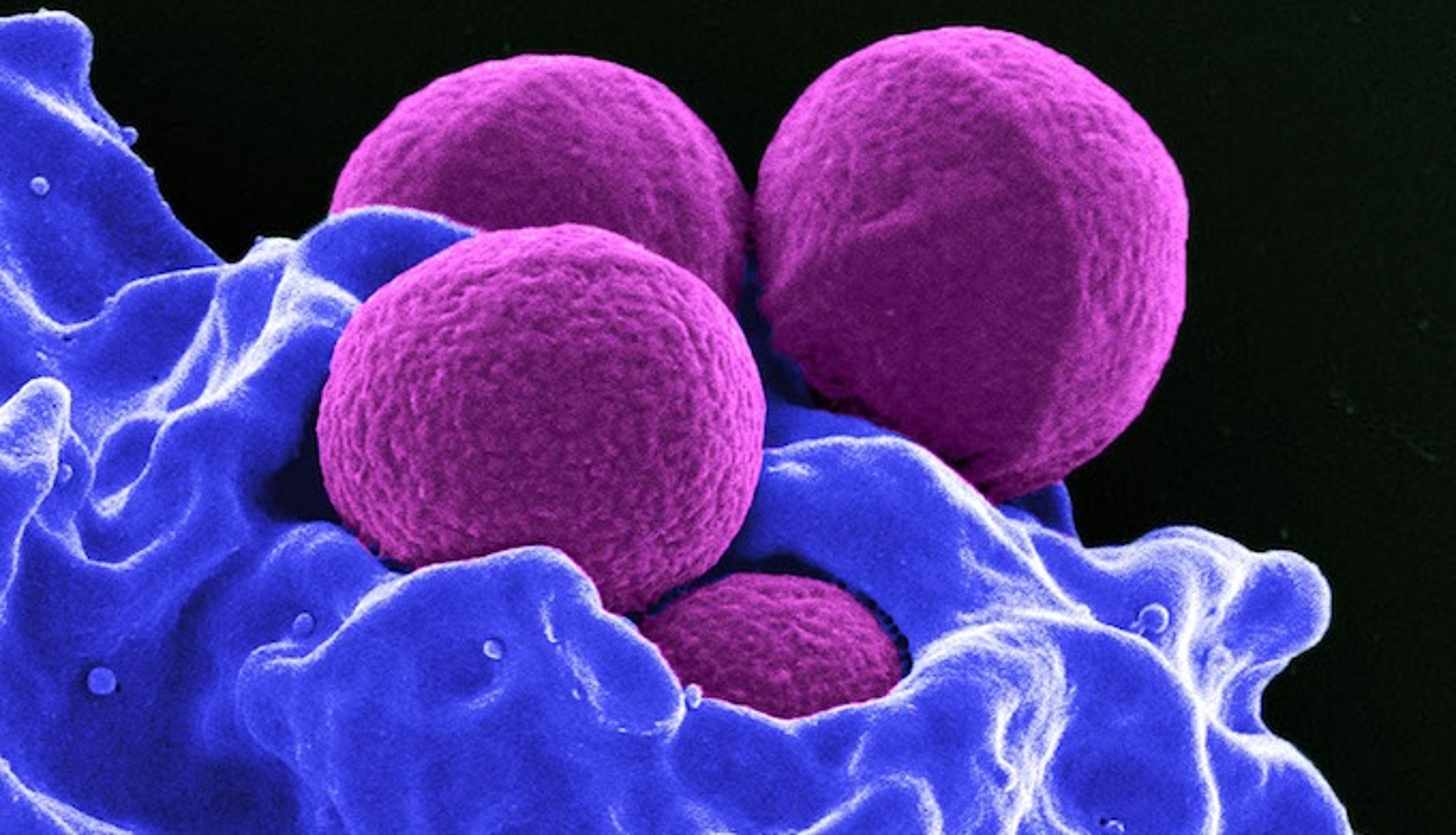
Antimicrobial resistance (AMR) is one of the biggest threats to world health. Experts warn that if action is not taken quickly, drug-resistant super bugs might result in millions of deaths annually by the year 2050. The ability to treat common infections is compromised by the growth of bacteria, viruses, and parasites resistant to medications, making routine treatments ineffective. This article examines the issue, its causes, ongoing actions, and future prospects in the fight against superbugs.
What does antimicrobial resistance entail?
The phenomenon known as “antimicrobial resistance” refers to how microorganisms (such as bacteria, fungi, and viruses) develop resistance to medications intended to kill them or stop their growth. This resistance develops over time, often as a result of excessive or inappropriate antibiotic use. The organisms that survive the use of these drugs have the potential to multiply, giving rise to ceppi that are more difficult, if not impossible, to treat with current therapies.
The reason for the antimicrobial resistance
Excessive use of antibiotics
One of the main factors that contribute to resistance is the inappropriate use of antibiotics, in both human and animal populations. The overuse of antibiotics, prescribing them when they are not necessary, and stopping treatments too soon are all behaviors that encourage the development of resistance.
Zootechnical settore
Massiccio utilizzo di antibiotici negli animali destinati all’alimentazione umana è un altro fattore. Antibiotics have frequently been used not only to treat illnesses but also to encourage animal growth. This results in a selection of resistant batteries that can be transferred to human beings through food or the environment.
The consequences of antimicrobial resistance
Morti prevenibili
According to some studies, antimicrobial resistance could result in up to 10 million deaths annually by the year 2050. Even infections that were once curable, such as polimonite or urinary tract infections, may become lethal if treatment is no longer effective.
Economic impact
Infections resistant to medications require more expensive and lengthy treatments, putting the world’s healthcare systems through a protracted trial. When compared to common infections, the expense of treating resistant infections is significantly higher. It is projected that by 2050, AMR might result in a 2-3% reduction in the global PIL
Current strategies to combat resistance
Creation of new pharmaceuticals
One of the most pressing challenges is the development of new antibiotics. However, the development of new drugs is a time-consuming and expensive process, and many pharmaceutical companies have given up on this field of research due to low profit margins.
Improvement of medical practices
It is imperative to manage antibiotics appropriately. This involves limiting the use of antibiotics in animals intended for release, educating patients on the significance of adhering to their treatment plan, and only prescribing antibiotics when necessary.
What are the international initiatives against antimicrobial resistance?
The International Organization for Health (OMS)
In an effort to tackle antibiotic resistance, the OMS has launched a global action plan that includes encouraging sustainable practices, funding research, and public education about the responsible use of antibiotics.
National Initiative
Numerose nation state have developed its own action plans to combat antimicrobial resistance, such as antibiotic stewardship, infection surveillance, and population-focused education campaigns.
What can each of us do to make a contribution?
Responsible use of antibiotics
It is essential that citizens use antibiotics only when prescribed by a physician and follow instructions to the letter. Never stop a treatment before it is finished, and never use antibiotics unless prescribed.
Prevention of infections
Adottare sempre le mani ragionevole, like lavarsi, può ridurre il rischio delle infezioni. Another crucial step in preventing the overuse of antibiotics is vaccination against infectious diseases that are common.
In conclusion
Antimicrobial resistance is a genuine and growing threat that necessitates coordinated worldwide action. Even if efforts are underway to develop novel treatments and improve the use of antibiotics, it is imperative that everyone play a role, from governments to single individuals. We can only hope to prevent a health crisis that could result in millions of deaths in the near future.
FAQ
1. What is antimicrobial resistance?
The ability of bacteria, viruses, and other microorganisms to withstand drugs that usually kill them or prevent their growth is known as antimicrobial resistance.
2. Quale sono le cauze principali dell’antimicrobial resistance?
The main causes include both improper and excessive use of antibiotics in humans and animals.Governments are developing action plans, encouraging the use of antibiotics sparingly and educating the public about the proper use of medications.
3. How can we prevent antimicrobial resistance?
Utilize antibiotici solo quando è necessario, adherere alla terapie prescritte in modo corretto e svolgere misure preventative like la vaccinazione and il lavaggio delle mani.
4. What are the consequences of antimicrobial resistance?
If left unchecked, antibiotic resistance could result in millions of deaths annually and have a catastrophic impact on global health systems and the economy.
5. What steps are the governments taking to fight
Governments are developing action plans, encouraging the use of antibiotics sparingly and educating the public about the proper use of medications.