Researchers have long flagged antimicrobial resistance as a public health concern, but this study is the first to analyze such trends around the world and over time.
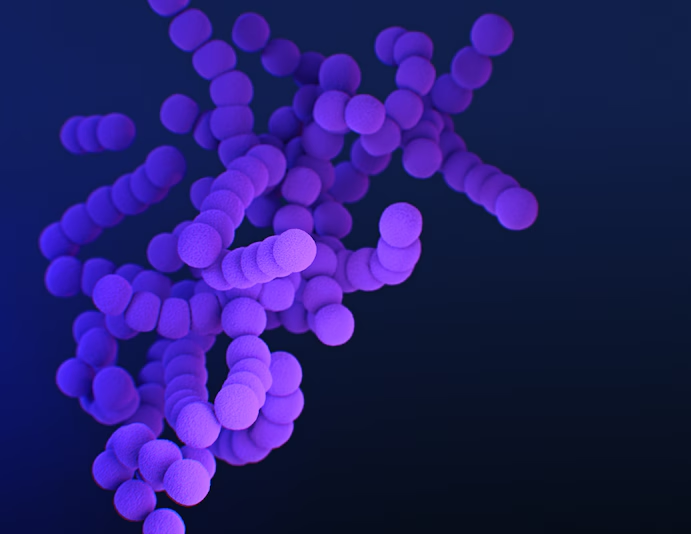
A Streptococcus bacteria that is resistant to a commonly prescribed antibiotic known as erythromycin. Group A Streptococcus bacteria can cause a variety of infections, from strep throat to pneumonia. (Meredith Newlove/Centers for Disease Control and Prevention)
| Main Topic | Subtopics |
|---|---|
| H1: Understanding the Impact of Antibiotic Resistance: A Global Crisis by 2050 | |
| H2: What is Antibiotic Resistance? | Definition and Overview |
| H3: The Science Behind Antibiotic Resistance | How bacteria evolve to resist antibiotics |
| H3: The Role of Antibiotics in Healthcare | Importance and application in treating infections |
| H4: How Misuse of Antibiotics Leads to Resistance | Overprescription and self-medication |
| H4: Global Health Threat: Projections for 2050 | Expected number of deaths and economic impacts |
| H3: How Antibiotic Resistance Affects Modern Medicine | Challenges in treating infections and surgeries |
| H4: Common Bacteria That Show Resistance | MRSA, E. coli, and other multi-drug resistant bacteria |
| H3: Antibiotic Resistance and Agriculture | Role of antibiotics in livestock and its effect on resistance |
| H4: Policies and Initiatives to Combat Antibiotic Resistance | WHO guidelines and governmental efforts |
| H3: Public Health Education and Awareness | How education can reduce misuse of antibiotics |
| H4: Alternative Treatments and Innovations | Research into new antibiotics and alternatives like phage therapy |
| H2: Case Studies of Countries Battling Antibiotic Resistance | Successful examples from Sweden, the Netherlands, and others |
| H2: The Future of Antibiotic Use in a Post-Antibiotic Era | Predictions for healthcare and new approaches |
| H3: Economic Implications of Rising Antibiotic Resistance | Impact on healthcare systems and global economy |
Understanding the Impact of Antibiotic Resistance: A Global Crisis by 2050
One of the biggest risks to public health that the world has ever faced is antibiotic resistance. If nothing is done, it is expected to result in 39 million fatalities by 2050, according to a report published in the Washington Post. This condition happens when bacteria develop defense mechanisms against medications intended to eradicate them, which results in inadequate therapy and potentially fatal illnesses.
Antibiotic resistance has far-reaching effects that go beyond personal health; it is a serious threat to economies, modern medical practices, and global healthcare systems. We need to learn more about the origins, effects, and preventative measures of the problem in order to fully appreciate its scope.
What is antibiotic resistance?
Antibiotic resistance occurs when bacteria change in response to the use of antibiotics, rendering them ineffective. This means that infections that were once easily treatable with common antibiotics become much harder, or even impossible, to cure.
Bacteria can acquire resistance through genetic mutations or by gaining resistance genes from other bacteria. Once resistant, these superbugs can multiply and spread, making it more difficult for doctors to manage infections.
The Science Behind Antibiotic Resistance
Resistance to an attack is a normal part of the evolutionary process. However, the overuse and abuse of antibiotics has sped up this process. When bacteria are treated with antibiotics, the weak ones die off, but the stronger ones survive and grow. This eventually creates a population of bacteria that the medications used to treat them are unable to eradicate.
The misuse of antibiotics in agriculture and healthcare is one of the main causes of resistance, but we’ll go into more detail about that shortly.
The Role of Antibiotics in Healthcare
Antibiotics are essential for treating bacterial infections, improving surgical site safety, and curing diseases like sepsis, pneumonia, and tuberculosis. They have revolutionized modern medicine by enabling medical professionals to cure serious infections that could otherwise be fatal and prevent infections during minor surgery.
Without efficient antibiotics, the success of routine operations, chemotherapy, and organ transplants could be considerably impaired.
How Misuse of Antibiotics Leads to Resistance
One of the main causes of antibiotic resistance is the improper use of antibiotics. This covers circumstances in which antibiotics are administered for viral diseases (such as the common cold), for which they are useless, or in which patients stop taking their prescriptions before the expiration date, allowing bacteria to proliferate and develop resistance.
Another factor is self-medication, especially in nations where antibiotics are freely accessible. When individuals take antibiotics without competent medical assistance, they may not use the recommended dosage or duration, further leading to resistance.
Global Health Threat: Projections for 2050
According to numerous studies and the World Health Organization (WHO), if substantial action is not taken to address antibiotic resistance, it may result in 39 million yearly deaths by the year 2050. This figure is concerning because it shows that antibiotic resistance poses a bigger risk to human life than cancer.
Devastating effects will also be seen economically, since the expense of treating resistant infections would put an excessive strain on healthcare systems. Prolonged disease and death that reduce productivity will have a significant impact on the world economy.
How Antibiotic Resistance Affects Modern Medicine
Numerous facets of contemporary medicine are under grave danger due to the emergence of antibiotic resistance. If effective antibiotics that are used to prevent and treat infections are no longer available, routine procedures like hip replacements, cesarean sections, and even dental work might become potentially fatal.
Antibiotics are essential for the health of patients with weakened immune systems, such as those receiving chemotherapy or HIV treatment. These people have a far higher chance of dying from infections without them.
Common Bacteria That Show Resistance
Several bacteria have already developed resistance to multiple antibiotics. Some of the most well-known examples include:
- Methicillin-resistant Staphylococcus aureus (MRSA): A type of staph bacteria resistant to several antibiotics.
- Escherichia coli (E. coli): A common bacterium that can cause urinary tract infections and other illnesses, some strains of which are now resistant to antibiotics.
- Carbapenem-resistant Enterobacteriaceae (CRE): A family of bacteria resistant to a class of antibiotics known as carbapenems, often used as a last resort for treating infections.
These resistant bacteria are more difficult to treat and often require stronger, more toxic medications, which can have severe side effects.
FAQs
1. What is antibiotic resistance?
Antibiotic resistance occurs when bacteria adapt to survive the antibiotics designed to kill them, making the drugs ineffective.
2. Why is antibiotic resistance a global issue?
It threatens the effectiveness of life-saving treatments and could lead to millions of deaths if no action is taken.
3. How does antibiotic misuse contribute to resistance?
Overuse and incorrect use of antibiotics allow bacteria to adapt and survive, leading to resistance.
4. What can be done to combat antibiotic resistance?
Efforts include better prescription practices, public health education, and developing new antibiotics.
5. Can antibiotic resistance be reversed?
Once bacteria become resistant, it’s difficult to reverse. The focus should be on preventing further resistance.
6. How does antibiotic resistance affect surgeries and treatments?
Without effective antibiotics, even routine surgeries could become risky due to the threat of untreatable infections.
Conclusion
Antibiotic resistance is an urgent global crisis that requires immediate attention. By understanding the causes, consequences, and potential solutions, we can work toward preventing millions of deaths by 2050 and preserving the effectiveness of these life-saving drugs.